- Arthritis
- Glenohumeral Debridement
- Anatomic Total Shoulder Arthroplasty(TSA)
- Reverse Total Shoulder Arthroplasty (RTSA)
- Hemiarthroplasty
- Ovo-Inlay Replacement
Arthritis
The loss of the smooth frictionless cartilage on the surfaces of the humeral head (the ball) and the glenoid (the socket) can cause pain, loss of motion, and progressive functional loss. Although not as common as arthritis of the hip or knee, shoulder degenerative joint disease (DJD) can be a source of significant pain and loss of function.
There are many causes of shoulder DJD:
Osteoarthritis: The “wear and tear” arthritis that occurs when the articular cartilage of the joint is no longer protecting the bones. This can cause the bones to migrate closer causing pain
Post-traumatic arthritis: Occurs when there is an injury that causes a shift is the environment of the shoulder. The initial injury, such as a fracture, could have resolved and healed, but it caused damage to allow arthritis to initiate.
Rheumatoid arthritis: An autoimmune disease that affects many joints causing severe pain and aggressive arthritis.
Rotator Cuff Tear Arthropathy: DJD due to a long stating rotator cuff tear that is no longer repairable.
Avascular necrosis of bone (AVN): A condition where blood is interrupted to humerus causing decay. This can be caused by an injury or predetermining factors.
Dr. Nicholson has been involved with designing shoulder replacement systems and has been involved extensively in researching outcomes of shoulder replacement techniques. His extensive knowledge and experience allows him to individualize treatment for each patient based on their condition, severity of joint damage, age, gender, activity level, expectations, and rotator cuff ability.
Severity
The severity of arthritis is split up into categories; mild, moderate and severe. Mild OA shows minimal changes on x-ray of the joint but can still cause intermittent pain, difficulty with range of motion and sleep disturbance. Moderate OA shows narrowing of the joint space, sometimes can cause clicking and grinding sounds and pain with motion. Severe OA often has grinding and crepitus throughout full range of motion, sleep disturbance and difficulty with activities of daily living.
It’s important to know the severity of arthritis to dictate conservative versus surgical intervention. Conservative treatment can begin with over the counter medications and physical therapy. Often steroid injections are attempted if pain persists after an attempt of oral medication. When all conservative treatment is no longer effective to alleviate pain, Dr. Nicholson often discusses what type of replacement would be best.

Glenohumeral Debridement
In cases of early or mild arthritis of the shoulder that have failed conservative management (medications, steroid injections, or physical therapy), a Glenohumeral Debridement may be surgical option.
An arthroscopic surgery involves using small tools and cameras to view the shoulder and is one of the least invasive procedures in orthopedics. A Glenohumeral debridement operation is an outpatient procedure to clean up some of the arthritis in the shoulder, restore balance and congruity, and improve pain and range of motion.
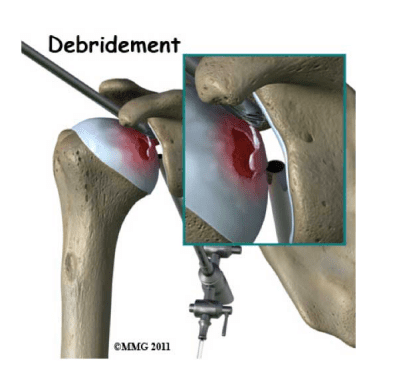
Recovery for this surgery involves 3-5 days in a simple shoulder sling, physical therapy for about 8 weeks and repeat evaluations every 4-6 weeks for 6 months. It does not cure or get rid of arthritis, but it can significantly reduce the symptoms of arthritis in a minimally invasive fashion.
For most cases, this procedure restores significant range of motion and decreases pain. Complications with this procedure is less than 1% due to infection, nerve damage, fracture and dislocations.
Total Shoulder Arthroplasty (TSA)
Candidates for a replacement surgery is recommended for patients with advanced arthritis (often referred to as “bone on bone”), when conservative management is not providing adequate relief.
An Arthroplasty, is another term for replacement. This surgery replaces both the ball and socket of the joint with a frictionless metallic ball and plastic socket. This provides frictionless pain free restoration of motion and function. A longer or shorter stem in the humerus is determined based on bone quality and determined on X-ray or CT scan. This is most appropriate when the rotator cuff is intact and functioning well.
This procedure is done through an open incision and is more invasive than an arthroscopy. It usually involves a 1-2 night inpatient stay in the hospital, but in selected patients can be performed as an outpatient procedure. Patients can expect to be in a sling for 4 weeks following the procedure and should participate in a physical therapy program to regain motion, strength, and optimal function for 12-16 weeks.
Patients with this procedure restore 95% pain relief and 90% of their age equivalent range of motion and strength.. Complications with this procedure is less than 1% due to infection, nerve damage, fracture and dislocations
For additional information in English, please click here
For more information in Spanish, please click here
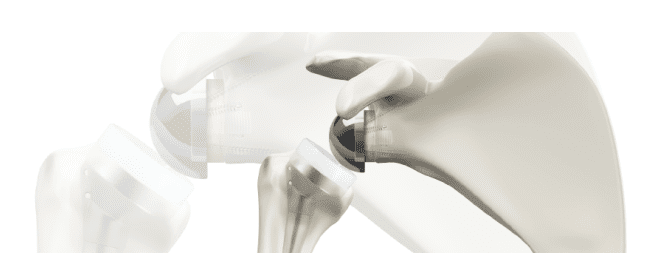
Reverse Total Shoulder Arthroplasty (RTSA)
Candidates for this type of shoulder replacement is most commonly used for patients diagnosed with rotator cuff arthropathy. Indications for a reverse total shoulder are expanding such as malunion fractures, revision of existing implants and failed rotator cuff repairs that cannot be re-repaired. Reverse Total Shoulder Arthroplasty is the best solution for these conditions because it utilizes the deltoid muscle to help elevate the arm rather than the rotator cuff. This surgery is more common for patients over the age of 70 because of the advantages of having a replacement that allows the rotator cuff muscle to be less demanding.
This type of arthroplasty reverses the orientation of the ball and the socket and alters the mechanics of the shoulder so that function can be restored without the presence of a rotator cuff. This procedure is done through an open incision and is more invasive than an arthroscopy. It usually involves a 1-2 night inpatient stay in the hospital. Patients can expect to be in a sling for 4 weeks and 90% of patients do home therapy.
Patients with this procedure can expect 95% pain relief. Patients every day function is significantly improved with activities of daily living and light sport activity. Complications with this procedure is less than 1% due to infection, nerve damage, fracture and dislocations.
For additional information in English, please click here
For more information in Spanish, please click here
Hemiarthroplasty (Hemi)
In certain situations, a hemiarthroplasty may be recommended, such as AVN (Avascular Necrosis). This surgery involves only replacing the ball (humeral head)of the humerus due to arthritis. Candidates for this surgery vary based on the diagnosis and current medical conditions such as but not limited to: a history of seizure disorder, acute humeral fracture without arthrosis and young patients.
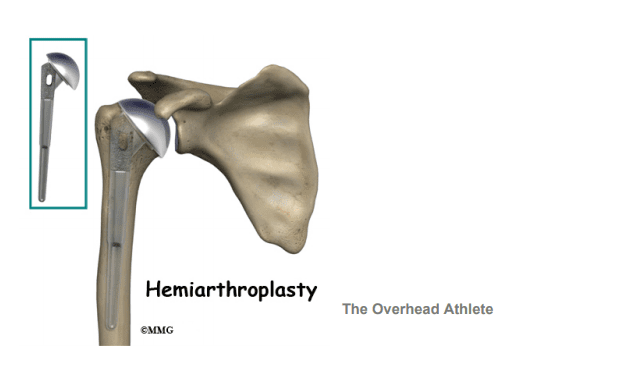
This procedure is done through an open incision and is more invasive than an arthroscopy. It usually involves a 1-2 night inpatient stay in the hospital, but some candidates can be out-patient based off of age and previous medical history. Patients can expect to be in a sling for 4 weeks and attend formal physical therapy from 8-12 weeks.
Complications with this procedure is less than 1% due to infection, nerve damage, fracture and dislocations.
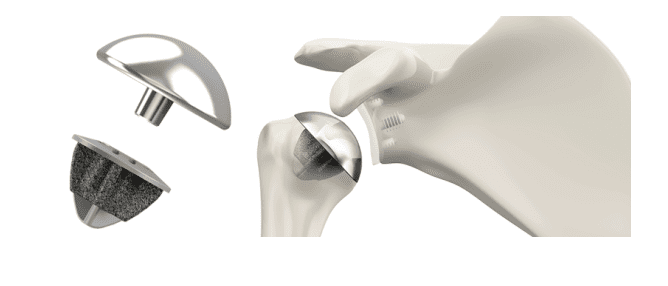
Ovo-Inlay Replacement
Patients who suffer from Shoulder Arthritis and wish to return to a high level of activity, may be a candidate for the Ovo-Motion Inlay-Glenoid Replacement. Most patients who are candidates for this type of surgery are under 70 years old.

This type of shoulder replacement allows for the least amount of native bone and cartilage removal to preserve the need for revision surgeries. Like traditional Total Shoulder Arthroplasties, both the glenoid and humerus are replaced to allow frictionless pain free motion and function. With the Ovo-Inlay, the humeral head (Ovo) is fitted and stem-less. The glenoid (inlay) component is plastic and allows for the return to weight bearing activity. For more information on this type of replacement, please click on the link, https://youtu.be/yPfH5OhKgM4
After surgery, patients are in a sling for 4 weeks and attend physical therapy for 12-16 weeks. Patients can expect to regain full range of motion within 2 months and return to all athletic activity between 3-5 months. Patients can expect 95% of pain relief and 90% of their age equivalent range of motion and strength. Complications with this procedure is less than 1% due to infection, nerve damage, fracture or dislocations.